Accountability Report
This section of the annual report will cover:
- Corporate Governance Report
- The risk and control framework
- Freedom to Speak Up
- System working and partnerships
- Organisation’s statutory obligations
- Review of economy, efficiency, and effectiveness of the use of resources
- Review of effectiveness
This section of the annual report will cover:
- Directors’ Report - Composition of the Board of Directors
- Scope of responsibilities and the risk and control framework
- Freedom to speak up
- System working and partnerships
- Review of economy, efficiency, and effectiveness of the use of resources
- Review of effectiveness
Directors’ Report - Composition of the Board of Directors
Chair: Malcolm Burch
Chief Executive:
Marie (Maz) Fosh (1 April 2023 – 31 July 2023);
Andrew Morgan (1 August 2023 – 31 March 2024)
Executive Directors and changes to appointments during the financial year:
- Professor Karen Dunderdale, Director of Nursing, Quality and AHPs and Deputy Group Chief Executive (from 1 August 2023)
- Sam Wilde, Director of Finance and Business Intelligence
- Dr Anne-Louise Schokker, Medical Director
- Ceri Lennon, Director of People, and Innovation (until 4 October 2023)
- Claire Low, Director of People and Organisational development (from 16 October 2023, non-voting board member)
- Reva Stewart, Chief Operating Officer (until 21 May 2023, non-voting board member)
- Julie Frake-Harris, Chief Operating Officer (from 10 July 2023, voting board member from November 2023)
Non-Executive Directors (NED) and Associate Non-Executive Directors (ANED) and changes to appointments during the financial year:
- Gail Shadlock, Doctors Disciplinary and Wellbeing Guardian Champion
- Ian Orrell, Audit Committee Chair
- Jim Connolly, Quality and Risk Committee Chair and Freedom to Speak Up NED Champion
- Murray Macdonald, Finance, Performance, People, and Innovation Committee Chair
- Rebecca Brown – Associate Non-Executive Director from 12 December 2023 (non-voting member)
Also, in attendance:
- Deputy Director of Corporate Governance
- Corporate Administration Manager and Personal Assistant
The Board met monthly throughout 2023/24 alternating between formal public and private meetings one month and board strategy, development, and training sessions the next. The Board’s main committees – the Quality and Risk Committee and the Finance, Performance, People, and Innovation Committee – met monthly. The Remuneration Committee met eight times during the year. The Board of Trustees for Charitable Funds met three times during the year.
Development of the Group Model governance arrangements
In 2022/23, our health and care system leaders commissioned an independent review of the Lincolnshire NHS provider landscape. The intention was to identify how providers can organise health and care to better meet the considerable service and financial challenges we face. The review said that Lincolnshire health and care system leaders should strengthen their ability to enable shared strategic and operational decision making to improve the delivery of integrated high-quality health and care.
Greater integration between Lincolnshire Community Health Services NHS Trust (LCHS) and United Lincolnshire Hospitals NHS Trust (ULHT) was one of the key recommendations. The review recommended establishing an NHS Trust Group arrangement between LCHS and ULHT, with the close engagement of other NHS partners.
Leaders felt that moving to a group model would most effectively address the issues of opportunity and urgency, and was the best model of provider collaboration to adopt because it would enable us to:
- balance greater organisational integration with the potential degree of disruption
- maximise the potential to integrate services and resources for the benefit of patients and to do this at pace
- address the most pressing patient harm issues and care integration opportunities
- supporting better use of resources and value for money
Through the year progression to a group model in April 2024 has been at pace, commencing with establishing a steering group at the end of quarter one, bringing both trust boards together in September through to the end of the year in a series of workshops to agree and define governance, financial, legal, digital and people workstreams. In November 2023 monthly board in common development sessions commenced to maintain the quoracy and sovereignty of both trust boards.
The quality committees in both trusts were identified in August 2023 to be the first sub trust board assurance committee to, through a series of workshops, map regulatory, legal and present Trust Board delegated authority and responsibilities, a quality committee in common in shadow form from January 2024. Through these workshops and collaborative discussions template agendas, terms of reference and workplans were agreed.
In quarter four the quality committee in common met each month receiving assurance from both trusts, enabling thematic review of complex patient safety, clinical effectiveness and patient experience and involvement risks, issues and good practice. Both trusts continue to maintain legal and regulatory compliance and assurance reporting, although coming together in a group model has enabled reduction in integrated urgent and emergency care treatment times, increased pace through collaboration of referrals between acute and community and improved and strengthened risk identification, mitigation and management across aligned portfolios and joint executive leadership.
Register of Trust Board Members Declaration of Interests – 2023/24
| Entry number | Name of employee | Official appointment in LCHS | Nature of interest (pecuniary or non-pecuniary) declared | Current interest | Date interest declared | Date recorded | Date interest ceased |
|---|---|---|---|---|---|---|---|
|
1. |
M Burch |
Acting Chair |
Chief Executive to the Lincolnshire Police and Crime Commissioner |
Yes |
26/6/2021 |
06/7/2021 |
|
|
2. |
M Fosh (left organisation on 31/7/23) |
Chief Executive |
Chair of the Urgent & Emergency Care Delivery Board
Co-Chair of the Lincolnshire Health & Care Collaborative |
No
No |
July 2020
25/10/21 |
02/03/21
18/11/21 |
31/07/23
01/01/23 |
|
3. |
S Wilde |
Director of Finance and Business Intelligence |
Member of the HFMA Costing for Value Institute Council
Chair – Community Services Reference Group – NHS Benchmarking Network
Co-chair of the NHS Benchmarking Network Steering Group |
Yes
Yes
Yes |
10/10/19
10/11/20
19/05/22 |
11/11/19
11/11/21
20/05/22 |
|
|
4. |
C Lennon (left organisation on 28/9/23) |
Director of People and Innovation |
Senior Responsible Officer – Lincolnshire People Board |
Yes |
Sept 2020 |
02/03/21 |
31/7/23 |
|
5. |
G Shadlock |
Non-executive Director |
Non-executive Director- Eastlight Community Homes |
Yes |
01/5/2022 |
03/5/22 |
|
|
6.
|
M Macdonald |
Non-executive Director |
Chief Executive to the Lincolnshire Housing Partnership
Chair of Manby Scouts Association
Patient representative at East Lindsey Medical Practice
Director – Humber Homes
Director – Boston Mayflower PLC
Chair – Greater Lincolnshire Housing Association Partnership
Non-executive Director – East Midlands Ambulance Service |
Yes
Yes
Yes
Yes
Yes
Yes
Yes |
1/7/2021
24/7/2021
24/7/2021
03/5/2022
03/5/2022
01/09/2022
12/12/23 |
06/7/2021
12/8/2021
12/8/2021
03/5/2022
03/5/2022
12/10/2022
13/12/23 |
|
|
7. |
J Connolly |
Non-executive Director |
Owner/Managing Director Riverside Consultants Ltd. – Provider of consultancy support to NHS and Adult Social Care
Owner/Director Riverside Coaching and Consultancy Ltd – Provider of Consultancy Support to Health and Social Care and Individual Coaching
Owner Jim Connolly Photography Ltd
Contractor of Services, as a vaccinator to K2 Healthcare.
Specialist Advisor - CQC
Wife is Associate Director of Nursing NHSE Midlands region |
Yes
Yes
Yes
Yes
Yes
Yes |
9/11/2021
9/11/2021
9/11/2021
9/11/2021
9/11/2021
9/11/2021 |
11/11/2021
11/11/2021
11/11/2021
11/11/2021
11/11/2021
11/11/2021 |
12/9/2023 |
|
8. |
R Stewart (left organisation 09/06/23) |
Chief Operating Officer |
SRO – Care Closer to Home portfolio |
No |
11/10/2022 |
11/10/2022 |
09/06/23 |
|
9. |
A-L Schokker |
Medical Director |
Emergency Care Improvement Support Team (ECIST) Regional Team session
GIRFT National Frailty team member |
Yes
Yes |
27/09/2022
01/02/2024 |
30/09/2022
06/02/2024 |
|
|
10. |
K Dunderdale |
Director of Nursing & Quality/Deputy Group Chief Executive |
Director of Nursing, United Lincolnshire Hospitals NHS Trust |
Yes |
17/10/2022 |
17/10/2022 |
|
|
11. |
I Orrell |
Non-executive Director |
Non-executive Director, Lincolnshire Partnership NHS Foundation Trust |
Yes |
8/3/2023 |
9/3/2023 |
|
|
12. |
J Frake-Harris |
Chief Operating Officer |
Interim Chief Operating Officer, United Lincolnshire Hospitals NHS Trust |
Yes |
11/12/23 |
22/12/23 |
|
|
13. |
A Morgan |
Group Chief Executive |
Chief Executive, United Lincolnshire Hospitals NHS Trust Partner member of Lincolnshire Integrated Care Board |
Yes
Yes |
01/08/23
12/9/2023 |
01/08/23
12/9/2023 |
|
|
14. |
C Low |
Director of People |
Director of People and Organisational Development, United Lincolnshire Hospitals NHS Trust
Interim Senior Responsible Officer for Lincolnshire |
Yes
Yes |
6/11/23
6/11/23 |
6/11/23
6/11/23 |
|
|
15. |
R Brown |
Associate Non-executive Director |
Non-executive Director, United Lincolnshire Hospitals NHS Trust |
Yes |
09/01/24 |
09/01/24 |
|
Scope of responsibility
As Accountable Officer, I have responsibility for maintaining a sound system of internal control that supports the achievement of the NHS trust’s policies, aims and objectives, whilst safeguarding the public funds and departmental assets for which I am personally responsible, in accordance with the responsibilities assigned to me. I am also responsible for ensuring that the NHS trust is administered prudently and economically and that resources are applied efficiently and effectively. I also acknowledge my responsibilities as set out in the NHS Trust Accountable Officer Memorandum.
The purpose of the system of internal control
The system of internal control is designed to manage risk to a reasonable level rather than to eliminate all risk of failure to achieve policies, aims and objectives; it can therefore only provide reasonable and not absolute assurance of effectiveness. The system of internal control is based on an ongoing process designed to identify and prioritise the risks to the achievement of the policies, aims and objectives of Lincolnshire Community Health Services NHS Trust, to evaluate the likelihood of those risks being realised and the impact should they be realised, and to manage them efficiently, effectively, and economically. The system of internal control has been in place in Lincolnshire Community Health Services NHS Trust for the year ended 31 March 2024 and up to the date of approval of the annual report and accounts.
Capacity to handle risk
LCHS has a comprehensive approach to risk management, accountability, ownership and responsibility of risks and issues. The risk management process is owned by Trust Board with Executive Directors and Deputy Directors being directly accountable for each risk and issue and for the appropriate and effective mitigating actions, in line with the Code of Governance, the NHS Provider Licence and the Orange Book, principles and concepts of risk management. The trust Risk Management Strategy outlines the responsibilities of the Trust Board, Executive Directors, Deputy Directors, the Deputy Director of Corporate Governance, senior leaders, and employees in accordance with roles, and the process of a monthly review of all Trust risks and the escalation process.
The Risk Management Strategy provides the overarching framework and guidance to enable this along with training and support provided by the Corporate Governance and Quality teams. Monthly assurance meetings discuss and review risks and issues, mitigations in place and learning from the management of these, which is shared through leaders across the Trust, the Trust Leadership team and extended leadership team discussions and in Trust Board Committees. The Deputy Directors, Divisional Leads, Heads of Service, Specialist Advisors and Quality Performance and Improvement Leads play a key role, individually and collaboratively, in effecting consistency in the assessment of risks and issues, the escalation and improvement of risks and issues and their subsequent movement onto and between LCHS corporate risk registers.
LCHS actively collaborates with partners across the Lincolnshire system to review and manage risks and issues proactively, collaboratively and collectively. Through the development of the group model, board in common and quality committee in common meetings in quarter four risk reporting has been strengthened, as seen by the pooling of support and resources across the Group to enable significant mitigations to integrated urgent and emergency care services, waiting list timeframes and mitigations of fire and estate risks.
On an annual basis, the Trust Board reviews the Trust Risk Appetite Statement along with examples of how this has been utilised in practice throughout the financial year to support decision-making. The 2023/24 Trust Risk Appetite Statement was aligned to the Trust’s strategic aims along with risk tolerance levels being set and aligned to strategic objectives as a further measure of risk management maturity and good practice to enable risk-based assurance discussions at committee and board level to focus on the more significant threats and opportunities requiring increased scrutiny, wrap around support and safety netting.
The Trust Risk Management Strategy has been reviewed by key stakeholders and risk champions within LCHS and proposed revisions have been discussed in assurance groups and Trust Committees prior to ratification by the Trust Board in March 2023 in preparation for the 2023/24 financial year. This included a full review and realignment of the Trust’s Risk Appetite Statement following board development sessions in-year and testing the 2023/24 risk appetite alignment to strategic objectives through Board decision discussions during the year.
The strategy is available to the public and employees on the Trust website. The purpose of the strategy is to ensure that risks and issues to the quality and delivery of patient services and care are managed to protect the services, reputation, and finances of the Trust, to create a culture where staff acknowledge risk as the responsibility of everyone and to ensure that the Trust meets its statutory obligations. The strategy defines the structures for the identification, management, ownership, review of risks and issues along with risk criteria, control and gaining assurance of risk or issue and the methods in which risks and issues are considered, assessed, and mitigated.
All risks with an overall score of 12 or above are noted on the Trust Corporate Risk Register are reviewed at least monthly by Deputy Directors in collaboration with Executives. Feeding into this is the Operational Risk Register for risks holding an overall score of 4 to 11, monitored through the Trust Leadership team monthly and informed by local risk registers held by divisions with support from Quality Performance and Improvement Leads and/or risk owners for corporate functions. Local risk registers for risks that have an overall score of 1 to 3 are owned by the risk lead and managed through local assurance groups. Robust mechanisms are in place to ensure risks are managed effectively, moved between registers appropriately and ensure sufficient time is allocated by each responsible committee or group for their consideration, review, and management. Through the risk identification process, staff at all levels can identify, assess, and develop mitigating action plans to reduce and manage each risk or issue effectively.
The organisation’s Risk Appetite Statement is published on the website and reviewed periodically through strategic decision-making application and the various risk registers are considered in its context.
The Trust Board is responsible for the management of key risks. The key areas of those risks are managed through:
- Corporate Risk Register (strategic, operational and local)
- Board Assurance Framework
- Financial risk management
- Compliance with targets
- Single Oversight Framework
- Operational Delivery Plan
- Performance management reporting
The Trust’s approach to corporate governance is rooted in best practice and is regularly reviewed and assessed through internal processes. While the strategy was collaboratively rewritten and published in March 2023, in preparation for the 2023/24 financial year, regular reports at every meeting of the Trust Board reflect developments, movements and mitigations of risks, issues and improvements to control arrangements. The Corporate Risk Register is reviewed and approved by the Trust Board as part of this process and in each public board meeting.
The risk management process has developed significantly through the year, through the development of the Trust risk tolerance alignment to strategic objectives. Additionally, the implementation of a more robust risk closure process ensuring the overall risk scores have been mitigated and managed for the score to be reduced to within the target and risk tolerance levels determined by Board. Regular Executive and Deputy Director workshops and huddles were introduced in August 2023 to strengthen mitigation action plans, risk and control management forming a key part of these discussions, have supported the development of the risk culture, and promoted collective as well as individual responsibility at the highest level and consistency in assessment.
A noteworthy development from April 2023 was to transition and support the Trust move from excel spreadsheet risk reporting to the Datix Web system. The Deputy Director of Corporate Governance and Quality Improvement and Performance Leads providing guidance and support to senior leaders and teams through quarters one and two to fully embed the new system and enable increased effectiveness, functionality, and reporting accuracy. In 2023/24 work commenced to align emergency preparedness responsiveness and resilience national risks to the Trust risk management processes and assurance structure.
The key high-scoring risks on the Corporate Risk Register during 2023/24 included the following:
- Risk of unmanageable community nursing staffing pressures which could result in patient harm due to inability to provide effective care when needed, an increased workload for staff and increased usage of bank, agency and overtime in addition to impacting on staff mental health and existing local care home pressures.
- There is a risk of harm to building occupants (including patients) caused by fire. There is a risk that the Trust cannot demonstrate statutory compliance in accordance with the Regulatory Reform (Fire Safety) Order 2005 (RRO).
- Risk that children and young people will wait much longer than usual for the treatment option of block of therapy intervention following assessment which could result in treatment delays, impact on patients’ mental health and social inclusion and in an increase in complaints and concerns received.
- Risk that the lymphoedema service will be unable to effectively manage their caseload and waiting list in terms of not being able to effectively assess and treat patients especially those who are complex and/or housebound. This could result in increased waiting times for patients, non-routine patients not being seen in clinic due to skill mix and a lack of skill development for staff.
- Risk of timely continence assessment and reassessments which may lead to patient harm and continence service will see an increase in routine patients waiting for assessment which is already substantially high.
- Risk to delivery of efficiency requirement and due to non-delivery of planned schemes, delays, or inability to implement efficiency savings of increased complexity due to system implications and potential reputational negative impact and ability to meet financial duties.
- Risk of inadequate ventilation in buildings due to dysfunctional plant systems and maintenance by third-party landlords resulting in potential disruption of services, adherence to infection prevention and patient safety.
Of the high-scoring risks from 2023/24 detailed above, mitigating actions for each risk continue to be implemented, such as the significant pooling of resource across the Group to act and mitigate at pace Trust estates, fire and ventilation safety and compliance works. Efficiency schemes were robustly managed throughout the year, the Trust demonstrating and achieving a break-even position at the end of the financial year. The remaining risks continue to be managed and reviewed regularly through the group-wide confirm and challenge risk review meetings to agree high and very high rated risks collaboratively.
Additional high-rating risks during 2023/24 that were closed or mitigated to the extent of movement to corporate operational or local risk registers were:
- Risk that demand exceeds workforce capacity at Gainsborough and Spalding Urgent Treatment Centres. Risk closed.
- Risk that the Trust fails to deliver all aspects of its financial plan due to service pressures, the level of demand being experienced and unforeseen events which could result in reputational damage, reduction in SOF rating and potential lack of sustainability. Risk closed.
- Risk of patient harm could be experienced due to prolonged periods of staffing shortages in community nursing, community nurses only have the capacity to attend to essential visits and operating on an OPEL 4. Risk closed.
LCHS is passionate about learning from risk management. In quarter four risk management transitioned from the portfolio of the deputy director of corporate governance to the quality team to align executive portfolios across the group model. Throughout the year the Deputy Director of Corporate Governance and Quality team have been working with teams and leaders across the organisation to provide advice about risk management, develop an understanding of definitions of risks and issues, the differences between controls for risk and actions to mitigate and supporting through coaching methodology.
The governance structure and Matters Reserved for the Board and Scheme of Delegation set out the route, responsibilities, and accountabilities of Trust Board, Committees and Specialist Groups for risk management and the escalation and improvement of risks and issues. The Board in Common and its committees have supported the development of risk and accountability ensuring corporate, operational, and local risk registers and the trust Board Assurance Framework shape each agenda has helped to embed the risk management culture of the Trust. Additional support to staff at all levels has been provided throughout the year to support identification, ownership of risk and appropriate escalation of risks and issues.
The Clinical Governance team is collaboratively developing a Group Risk Management Policy and process building on learning and risk maturity from both trusts, which will continue to progress through 2024/25.
There is a robust Board Assurance Framework in place which sets out the key controls and assurances on controls to safeguard against the key risks to the achievement of the strategic aims and objectives. The Board Assurance Framework is aligned with the organisation’s Operational Plan and is reviewed at every meeting of Trust Board and its assurance committees. In addition, there are formal risk management procedures in place with effective review and management procedures which incorporate both a controls assurance and a risk assessment.
The committees of the Trust Board – the Quality and Risk Committee (QRC), and in quarter for the Quality Committee in Common; and the Finance, Performance, People, and Innovation Committee (FPPIC) – assess every business item against the Board Assurance Framework and the Trust’s noted appetite for risk for each strategic aim. This enables direct assessment against compliance on all fronts, including the Care Quality Commission (CQC) requirements. The committees review the corporate risk register monthly, with an overall score of 12 or above, in addition to risks on the operational risk register, with an overall score 4-11, where the Trust risk appetite is noted as ‘cautious’. The Trust has a cautious risk appetite for risks and issues relating to patient safety or harm, staff safety and wellbeing, cyber security, health and safety and recruitment compliance. Board members agreed when reviewing and setting the 2023/24 risk appetite that upward reporting from committees to Board will identify such risks that require Board’s attention on the operational risk register.
The Risk Management Strategy and the Trust Governance Manual (Standing Orders, Standing Financial Instructions and the Matters Reserved to the Board and Scheme of Delegation) stipulate the accountability for risk management and approval of changes to the Corporate Risk Register lies with the Trust Board. Operational management and oversight for the Operational Risk Register (ORR) resided with Trust Leadership team until May 2023, where the decision was taken for all risks to report through the committee assurance structure. In September 2023 the Executive Leadership team commenced meeting together, moving in November to a Group Executive Leadership team (ELT) at which point key risks commenced being escalated into ELT.
Separately, the People Executive Group (PEG), chaired by the Executive Director of People, has delegated responsibility for ensuring the Trust has developed and managed the short, medium and long-term workforce strategies and staffing systems to progress delivery with the national People Promise planning and recommendations. In addition, PEG has provided People Strategy and People Plan progress reports, assurance reports and update risk and work plans to FPPIC. All policies approved by this forum can be escalated to Board for endorsement and/or challenge. Quality and Equality Impact Assessments are completed to assess substantive changes to the workforce or services and are reviewed and approved through the Quality and Equality Impact Assessments Panel, which reports to Quality and Risk Committee, and in quarter four the quality committee in common. As a pilot Equality Delivery System (EDS) 3 site in 2022/23, the Trust completed implementation of the EDS3 framework into business as usual programmes.
The Digital Executive Group (DEG) holds delegated responsibly and oversight for digital, cyber and information governance and data privacy, continuing in year to significantly develop and strengthen the trust position in relation to cyber and digital security and opportunities for developing patient care provision in the home.
Sharing the learning gained through risks and issues, incidents, complaints and claims management processes is an essential component of maintaining the risk management culture within the trust. Learning is shared through divisional and corporate structures and trust-wide governance committees and groups as outlined in the Trust’s organisational structure. Assurance and learning conversations take place in local assurance groups, such as the Quality Assurance Groups that support each clinical division, and report to specialist groups like the Stakeholder, Engagement and Involvement Group, Learning from Deaths, Drugs and Therapeutics Group and the Health and Safety Committee.
Learning is acquired from a variety of sources that include:
- analysis of incidents, complaints, claims and acting on the findings of investigations
- quality impact assessments
- equality impact assessments
- equality delivery system
- freedom to speak up
- non-executive champions
- external Inspections
- internal and external audit reports
- clinical audits
- outcome of investigations and inspections relating to other organisations.
Our Freedom to Speak up Guardian (FTSUG) is well embedded in the Trust and plays a lead role in engagement and interaction with our staff. This role supports the organisation in complying with the outcomes set up by the National Guardian Office (NGO) and the outcomes include:
- A culture of speaking up is instilled throughout the organisation.
- Speaking up processes are effective and continuously improved.
- All staff have the capability to speak up effectively and managers have the capability to support those who are speaking up.
- All staff are supported appropriately when they speak up or support other people who are speaking up.
- The Board is fully sighted on, and engaged in, all Freedom to Speak Up matters and issues that are raised by people who are speaking up.
- Safety and quality are assured.
Our FTSUG works hard to ensure the NGO values and principles of speak up are embedded in their work, these are:
- Courage: speaking truthfully and challenging appropriately
- Impartiality: remaining objective and unbiased
- Empathy: listening well and acting with sensitivity
- Learning: seeking and providing feedback and looking for opportunities to improve.
The NGO in partnership with NHS England has produced a new and comprehensive Freedom to Speak up Policy for the NHS, which was amended for local requirements and published on the LCHS website in January 2024.
https://www.lincolnshirecommunityhealthservices.nhs.uk/download_file/242/189
NHS England and the National Guardians Office are auditing, and compliance outcome is given via the National Guardians office portal.
Response to the trial and conviction of Lucy Letby
LCHS FTSUG made a bespoke statement in communications pertaining to our organisation and gave staff a reminder of how we all need to raise any matters that impact on the care our patients deserve.
Amanda Pritchard Chief Executive NHS wrote to all NHS trusts following the convictions requesting each Trust ensures the following.
| Requirement | LCHS Action/Response |
|---|---|
|
All staff have easy access to information on how to speak up. |
All staff have access via induction, intranet, internal social media posts and corporate communications. |
|
Relevant departments, such as Human Resources, and Freedom to Speak Up Guardians are aware of the national Speaking Up Support Scheme and actively refer individuals to the scheme. |
All are aware of the speak up support scheme and it is included in policy - no referrals have been made due to very low detriment levels and those that do report every effort is made to resolve the issue and have not felt the requirement for the scheme. |
|
Approaches or mechanisms are put in place to support those members of staff who may have cultural barriers to speaking up or who are in lower paid roles and may be less confident to do so, and those who work unsociable hours and may not always be aware of or have access to the policy or processes supporting speaking up. Methods for communicating with staff to build healthy and supporting cultures where everyone feels safe to speak up should also be put in place. |
FTSUG attends staff networks and has champions in the networks, makes visits out of 9-5 and on teams after hours, speak to all levels on site visits, e.g., housekeeper, volunteers, students on placements bank and agency staff, contractors.
|
|
Boards seek assurance that staff can speak up with confidence and whistle-blowers are treated well. |
Detriment cases are escalated and reported to the NED & CEO, plus feedback from contacts is included in reports to service leads, both positive and negative. |
|
Boards are regularly reporting, reviewing, and acting upon available data. |
FTSUG provides six monthly reports to board in person so challenge and scrutiny can occur. 1:1 with NED responsible for speak up is undertaken quarterly and ad hoc as required. |
The 2023 National Staff survey showed a small decline in all four of the speak up questions and this will be formally presented to the board and executives to formulate an action plan.
Summary of Contacts to Speak up Guardian
The Guardian had 88 contacts in the defined period 2024/24. The trend being static now for three years. Eight of the contacts were from exit questionnaires.
One contact was from an anonymous source which would indicate less fear of detriment and confidence in the guardian’s ability to maintain anonymity also speak up perceived as more business as usual.
One case of disadvantageous treatment resulting from speaking up has been raised, this was rapidly escalated and investigated, resulting in a large piece of work involving the patient safety team and involvement of the relevant director and non-executive director responsible for speaking up.
15 of the contacts have left the organisation, 13 for the reason pertaining to the speak up.
Ten of the 24 contacts from inpatient wards were from one specialised area and has been flagged as requiring culture/engagement work. Two were from staff working on United Lincolnshire Hospitals NHS Trust (ULHT) wards the remaining from LCHS community hospitals.
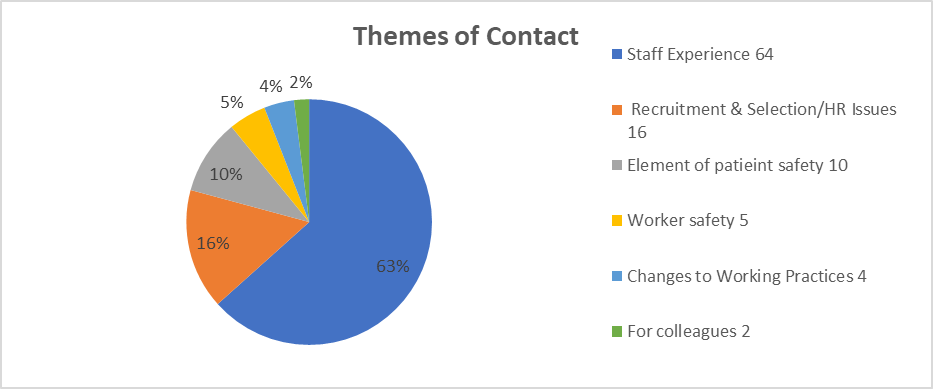
Note: ‘Staff Experience’ includes behaviours, bullying, relationships and working conditions. 19 of the 64 contacts used wording “bullying and/or harassment” – no cases were raised formally.
‘Worker safety’ includes health & safety at work and emotional wellbeing issues.
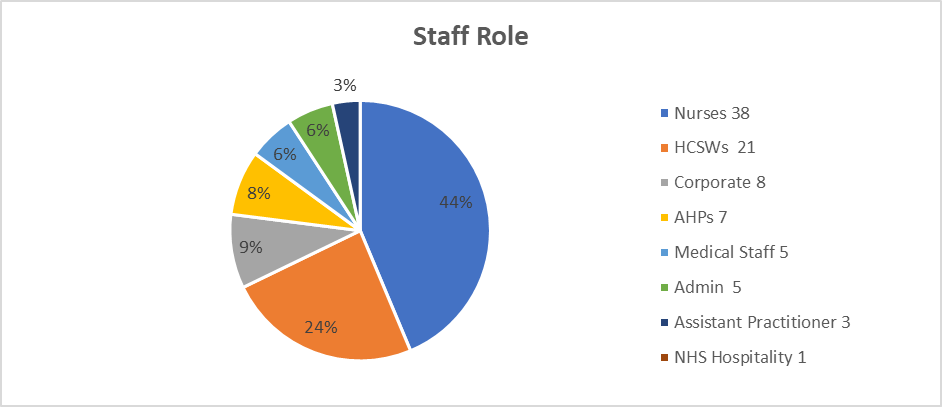
Note: 22 of the contacts were band 7 or above.
Nurses continue to be the largest number but represent a larger portion of the workforce.
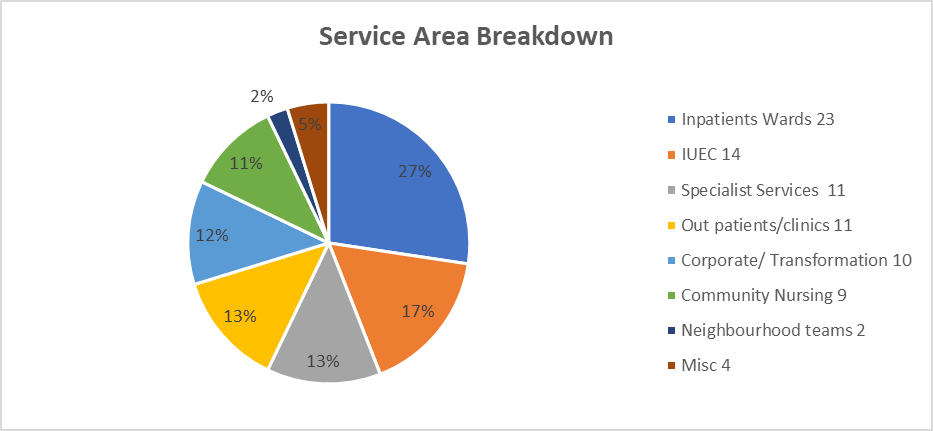
Miscellaneous - Single contacts came from – Finance Business Intelligence, Mass Vaccination, Medicine Management and NHS property - porters.
|
Summary of FTSUG Activity |
Action/Outcome/Narrative |
|---|---|
|
HR/Recruitment & working practices |
There were 20 contacts in this category. The FTSUG mainly signposted these to other areas such as unions or encouraged open dialogue with those concerned. The majority were resolved by informal means but with the importance of communication and rationale to contacts would have prevented these issues. This has been raised with senior leaders in the operational delivery group and emphasis requested on leaders building trustful relationships with their staff avoiding suspicion and an oppositional standpoint. |
|
Community Nursing Teams including community HCSW’s.
|
There has been a noticeable decline in the contacts from community nursing teams, the rationale being unclear but analysis and discussion with groups has deduced the following:
During visits staff do not want to be formally identified as speaking up but use the opportunity to have themes communicated and place trust in the FTSUG to ensure this occurs. This has increased the reach of the speak up process but not necessarily shown a difference in contact numbers, however, would indicate a more” business as usual” approach. |
|
Staff Experience |
The largest number of contacts remain staff experience – mainly poor relationships in teams or with leaders, seemingly unfair treatment, incivility. 19 contacts used the words bullying and/or harassment in their dialogue with the FTSUG, these did not escalate into formal processes. Areas that had previously shown high levels of dissatisfaction with staff experience have noticeably decreased in contacts (IUEC) – leaders in this division have interacted in a positive way with the FTSUG and sought advice and support in styles of leadership and approaches. |
|
Managers seeking advice to facilitate an improved culture. |
During the report period 13 leaders have requested advice on dealing with issues in their area to ensure they are dealing with staff in a way that underpins all the values of openness and freedom to speak up. This has demonstrated a willingness to learn and a trend towards open leadership. The FTSUG has supported leaders with guidance and materials to assist. There are still occasional concerning responses to speak up and these are escalated to the line manager of those concerned. |
|
Patient Safety/Quality Issues 10 contacts |
Where elements of quality and safety issues were raised these are escalated rapidly. Two of the contacts were pertaining to one area and involved patient acuity which was escalated to medical director level. A further contact was pertaining to standard operating procedures, and this was fully investigated by the patient safety lead – with outcomes being overseen by the Deputy Director of Operations & Nursing & Director of Nursing. Other patient safety issues were around staffing levels.
|
|
Protected characteristics.
|
The FTSUG has continued to collate the EDI factors, 16 of the 88 contacts had protected characteristics. (18%). Contact with FTSUG also enabled the Staff Health Passport to be promoted to very positive feedback. There have been no contacts from our new staff who have been recruited from overseas, contact has been made in groups and individually with these staff to promote the speak up agenda and its value in the UK health systems. |
The backdrop for year one of the FBI Strategy is a complex environment in flux. Playing an active role in the Lincolnshire Integrated Care System (ICS) continues to present opportunities and challenges through its structures and processes including:
- The Integrated Care Strategy which describes how the Integrated Care Partnership will meet the health and care needs of the Lincolnshire ICS footprint
- The Integrated Care Board 5-year Joint Forward Plan which defines the role of the NHS in delivering the strategy
- A new system operating plan for 2023/24
- The Strategic Delivery Plan intended to restore financial balance in the system
- The Provider Collaborative and its role in service transformation
- The Lincolnshire system provider review
- An expected refresh of the 5-year Lincolnshire Long Term Plan.
Organisation’s statutory obligations
The trust is fully compliant with the registration requirements of the Care Quality Commission, Secretary of State, NHS England and statutory regulators of health care professions ensuring compliance is reviewed, monitored and reported and acted upon through the trust governance and assurance structure.
The trust has published on its website an up-to-date register of interests, including gifts and hospitality, for decision-making staff (as defined by the trust with reference to the guidance) within the past twelve months, as required by the ‘Managing Conflicts of Interest in the NHS’ guidance.
As an employer with staff entitled to membership of the NHS Pension Scheme, control measures are in place to ensure all employer obligations contained within the Scheme regulations are complied with. This includes ensuring that deductions from salary, employer’s contributions and payments into the Scheme are in accordance with the Scheme rules, and that member Pension Scheme records are accurately updated in accordance with the timescales detailed in the Regulations.
Control measures are in place to ensure that all the organisation’s obligations under equality, diversity and human rights legislation are complied with.
The Trust has undertaken risk assessments on the effects of climate change and severe weather and has developed a Green Plan following the guidance of the Greener NHS programme. The trust ensures that its obligations under the Climate Change Act and the Adaptation Reporting requirements are complied with.
The Trust monitors climate related issues through the approved Green Plan. Reporting on activities, achievements, targets and developments are reported to the Trust subcommittee on a quarterly basis formally, issues or updates can be raised at the Group Leadership Team forum, held monthly.
Additionally, climate related issues are measured through the Trust’s overall Operational Delivery Plan, where the Green Plan forms a major part of that overall Trust strategy. Key performance indicators are listed and monitored through the plan and is reported monthly to the Trust Board.
Additional reporting metrics, flow through to the board via ERIC, PAM and the Greener NHS Data Collection which all are signed off by the Trust Board annually.
Climate related issues are largely but not exclusively monitored through the Estates, Facilities and Innovation directorates, and encompass many of the management structures within.
The Estates management structure has specific reasonability for sustainability, energy usage and reduction. The dedicated sustainability manager holds the responsibility under the Trust Board within the Estates and Facilities directorate for all climate related issues.
The capital management structure incorporates the latest climate related legislation, guidance and good practice in any new build or major refurbishment within the design phases.
The Facilities management structure has specific responsibility for the Trust’s travel plan where a range of initiatives covering vehicular usage, EV use, cycle schemes and wider schemes such as those relating to landscaping, through natural wild gardens and tree planting for new capital schemes.
All management structures report weekly into the Estate and Facilities senior management team, this then is reported through the FPPIC procedure into the Trust board on a quarterly basis.
Internally the Trust has a weekly communication strategy, via email and Intranet available to all staff members which updates collectively on relevant climate related issues, progress on our net zero carbon strategy and regularly promotes energy reduction initiatives.
Information governance
There were no Personal Data Breaches reported to the Information Commissioner’s Office (ICO). The Digital Executive Group (DEG) oversees all Information Governance and Data Protection issues and reports to the Finance, Performance, People, and Innovation Committee whilst also providing assurance to the Trust Board to ensure that legal, statutory, and regulatory requirements are met.
The DEG is chaired by the Senior Information Risk Owner (SIRO), who is the Chief Operating Officer (COO). Staff are encouraged to report incidents and seek further advice and guidance regarding any additional actions that may require implementing.
Mandatory information governance (IG) training follows the Core Skills Training Framework (CSTF) and is an annual requirement for all staff. Induction training for new starters is delivered through the accredited e-learning ‘Data Security Awareness Training’ which requires a minimum pass of 80%.
Staff are governed by a code of confidentiality for any data they have access to which is strictly access controlled through National Policy and Role Based Access Control (RBAC). Each information system, whether corporate or clinical, has a designated Information Asset Owner (IAO) with defined responsibilities, including risk management. These are supported by Information Asset Administrators (IAO) at a local level.
The publication for the Data Security and Protection Toolkit (DSPT) was on 30 June 2023. The internal audit report achieved ‘Significant Assurance’ with some improvement required.’ This level of assurance has been achieved for four consecutive years.
Data quality and governance
The Business Managers within the Finance and Business Intelligence Directorate conduct regular data quality checks on datasets and reports. The team connects with the national NHS Benchmarking work which enables the trust to benchmark its own data with that of other trusts to enable comparators and scope for improvement. The team works closely with the Digital Health team to enable front-end changes to correlate into meaningful data and analysis. The team also provide key data that informs Performance Management Reviews, which are conducted with each division and corporate area to assess performance against agreed key performance indicators and metrics to drive measurement, review, and improvement.
Performance data and reporting is a key component of FPPIC and Quality and Risk Committee (QRC), and since January 2024 the Group Quality Committee in Common assurance, highlighting areas where key performance indicators and metrics are being achieved and can be celebrated, or enable committees to focus attention to inconsistent performance or where indicators are not being achieved and to prompt appropriate action to be taken.
Key FPPIC performance indicators relate to our people, recruitment, health and safety, digital programmes, access and tackling digital inequalities, strategic planning, partnership working and feedback from commercial stakeholders and financial planning.
The Quality and Risk Committee, and since January 2024 the Group Quality Committee in Common, considers a wealth of performance information from complaints, incidents, safeguarding contacts and referrals, compliments, claims received, national Quality Board data, patient friends and family test percentage responses through to collating lessons learned following feedback and demonstrating the impact of acting on feedback and learning in service developments.
As Accountable Officer, I have responsibility for reviewing the effectiveness of the system of internal control. My review of the effectiveness of the system of internal control is informed by the work of the internal auditors, clinical audit and the executive managers and clinical leads within the NHS trust who have responsibility for the development and maintenance of the internal control framework. I have drawn on the information provided in this annual report and other performance information available to me. My review is also informed by comments made by the external auditors in their management letter and other reports. I have been advised on the implications of the result of my review of the effectiveness of the system of internal control by the board, the audit committee [and risk/ clinical governance/ quality committee, if appropriate] and a plan to address weaknesses and ensure continuous improvement of the system is in place.
As the Accountable Officer, I have the responsibility for reviewing the effectiveness of the system of internal control. My review of the effectiveness of the system of internal control is informed by the work of the internal auditors, clinical audit and the executive managers and clinical leads within the NHS Trust who have responsibility for the development and maintenance of the internal control framework.
I have drawn on the information provided in this annual report and other performance information available to me. My review is also informed by comments made by the external auditors in their management letter and other reports. I have been advised on the implications of the result of my review of the effectiveness of the system of internal control by the Board, the Audit Committee, the Finance, Performance, People and Innovation Committee e and the Quality and Risk Committee, transitioning to the Group Quality Committee in Common, as well as sub-committees and others within the group structure, and a plan to address weaknesses and ensure continuous improvement of the system is in place.
My review is informed in a number of ways. The Head of Internal Audit provides me with an opinion on the overall arrangements for gaining assurance through the Board Assurance Framework and on the controls reviewed as part of the internal audit work. Executive managers within the organisation who have responsibility for the development and maintenance of the system of internal control provide me with assurance. The Board Assurance Framework itself provides me with evidence of the effectiveness of controls that manage risks to the organisation.
My review was also informed by:
- delivery of audit plans by external and internal auditors
- unconditional registration with the Care Quality Commission.
The Head of Internal Audit is required to provide an annual opinion on the systems and processes of internal control employed in the trust. The Head of Internal Audit Opinion provided a rating of Reasonable Assurance, the second highest rating to be awarded.
During the year the trust has made real and sustainable improvements to its control and governance arrangements. It has embedded further structure and guidance in relation to the understanding and management of risk and clinical audit and further improvements to re-align and enhance its governance arrangements relating to patient safety, fire and estates safety, equality, diversity and inclusion and to reduce health inequalities and digital inequalities.
Audit Committee
The Audit Committee meets quarterly and has a key role in providing assurance to the Trust Board on the control mechanisms that are in place across the trust. The Audit Committee reviews the adequacy of all risk and control-related disclosure statements together with any accompanying head of internal audit statement prior to endorsement by the Trust Board. The committee receives regular update reports from, among others, the Director of Finance and Business Intelligence, the Deputy Director of Corporate Governance and both internal and external audit.
During the year the Committee gave particular consideration to the developmental areas highlighted to trust through internal audits completed during the year with relevant leads in the trust providing follow-up assurance of completion of actions and improvement realised, such as the significant positive reduction of cyber security, financial planning and break-even. LCHS continued to develop the vaccination centre and mobile provision of covid and flu vaccinations in addition to health promotion support to vulnerable groups, homebased patients and in collaboration with primary care colleagues commence the rollout of the measles vaccines through the centres and model for Easter 2024.
The committee continues to develop and enhance mechanisms to gain assurance on all areas that come within its terms of reference, which were also reviewed and amended during 2023-24. It approves a programme of work by internal audit (TIAA), external audit (Mazars LLP) and counter fraud, based on risk analysis and clinical assurance mechanisms, to allow it to provide the necessary assurance to the Trust Board on an on-going basis.
Names of directors forming an audit committee
- Ian Orrell – Chair
- Gail Shadlock – Non-Executive Director
- Rebecca Brown – Associate None Executive Director, commencing with the trust on 12 December 2023.
Also, in attendance:
- Deputy Director of Finance, Performance, and Information
- Deputy Director of Corporate Governance
- Medical Director/ Deputy Medical Director
- Client manager (internal audit)
- Director (external audit)
- Local Counter Fraud Specialist.
Quality and Risk Committee (QRC)/ Quality Committee in Common
The Quality and Risk Committee met each month, other than in December when the committee was stepped down by virtual means. From January 2024 the Quality Committee in Common commenced meeting across the group model, maintaining quoracy for both LCHS and ULHT. The Committee provides assurance to the Trust Board that appropriate and effective clinical and quality governance mechanisms are in place for all aspects of quality and risk including safety of clinical services, management of risk, understanding and acting on patient feedback, clinical effectiveness including health outcomes, learning from incidents and complaints, clinical audits, NICE guidance and review, medications management and medical devices, delivery of the Clinical Strategy, equality, diversity, inclusion and health inequalities (access to services, impact of change on patients and the public), population health management, verbal updates, as necessary, from Non-Executive Director Champions (Freedom to Speak Up and Doctor’s Disciplinary), compliance with national, regional and local regulatory requirements.
Finance, Performance, People and Innovation Committee (FPPIC)
The committee provides assurance to the Trust Board that appropriate and effective governance mechanisms are in place for all aspects of financial and operational strategy, policy, management and reporting, people and innovation, health and safety, performance management and reporting, procurement strategy and investment policy, integrated business planning, associated strategies, digital health and cyber security, security management, information governance, equality, diversity, inclusion and health inequalities, population health management (performance, finance, data and staff aspects), verbal updates, as necessary, from Non-Executive Director Champions and compliance with national, regional and local regulatory requirements.
The committee has provided effective challenge and assurance in oversight for strategic aims 3, 4 and 5, particularly relating to vacancy and recruitment developments, inclusive of international recruitment, financial accountability, planning, delivery and performance, such as the change of ledger provider and support infrastructure; development of business intelligence in addition to estates, innovation and digital developments.
Trust Leadership Team
The Trust Leadership Team (TLT) continued to meet throughout the year. TLT comprises of executive directors, deputy directors and divisional leads. TLT oversee the running of Trust business and connect into committees and the Trust Board as required. The team also hold responsibility for the corporate operational risk register until May 2023.
Executive Leadership Team
The Executive Leadership Team (ELT) commenced meeting together in August 2023 and jointly across the group from November 2023. ELT meets weekly as accountable executives and is the business decision-making meeting for business items, discussions and shaping proposed direction to the Trust Board.
Progression of the group model in 2024/25 continues with the recruitment of the group executive team, learning from the group quality committee in common from quarter four of 2023/24 being taken forward to develop a group people committee and governance structure to support finance, performance and transformation with system partners.
In conclusion, I am assured that no significant control issues existed within the Lincolnshire Community Health Services NHS Trust during the 2023-24 year.
Signed: Andrew Morgan Date Signed: 30/06/2024
Accountability Report page list
-
This section includes the Chief Executive and Chair’s Foreword for the year 2023/24.
-
This section of the annual report will cover: Performance overview by the chief executive, performance overview, about us, summary of our structure and services provided, our strategic aims and objectives 23/24, the LCHS Way, LCHS 2023/24 key facts and figures, our achievements during 2023/24, Lincolnshire NHS Charity, the future: looking ahead to our strategies for 2024/25, going concern and quality priorities
-
This section of the annual report will cover: Corporate governance report, the risk and control framework, Freedom to Speak Up, system working and partnerships, organisation’s statutory obligations, review of economy, efficiency, and effectiveness of the use of resources and review of effectiveness
-
This section of the annual report will cover: Remuneration report and staff report
-
This section includes LCHS's annual accounts for the year ended 31 March 2024.
